You are here
出版物 & 研究
出版物 & 研究
出版物 & 研究
香港賽馬會災難防護應變教研中心的出版物涵蓋了教研中心跟合作夥伴、顯赫學術機構的研究項目,以及有關災難防護和應變的其他研究與開發。
指引列出了教研中心特別揀選的災難管理技術資訊、操作指引和有用工具。
博客提供了一個平台,讓持份者能分享與災難有關的最新動態、意見及經驗分享。
博客文章由作者以個人身份或代表所屬單位撰寫。內容表達的觀點、思維及意見純屬作者個人想法,並不代表香港賽馬會災難防護應變教研中心的立場。
公眾可在尊重知識產權情況下,使用所有資料,並必須適當引述出處。
2020

[本文只供英語版本]
[本文只供英語版本]
7 November, 2020
It seems that COVID-19 will be more active in winter as seen by the increasing incidence in many countries in northern hemisphere. Unfortunately, seasonal influenza typically shows a spike from November to March in the Northern Hemisphere and from June to August in the Southern Hemisphere, coinciding with cold weather conditions. Therefore, we may face double troubles in winter times. That’s why we need to understand more about the behaviours of these two types of viruses. The World Health Organization (WHO) has issued warning on the co-circulation of influenza and COVID-19. Both of them cause respiratory disease and that could place an additional burden on vulnerable populations and healthcare systems that are already stretched because of the COVID-19 pandemic.

Photo Source: South China Morning Post (scmp.com)
There are concerns about the overlap of the flu season with the COVID-19 pandemic, coupled with the similarities of the two viruses. Firstly, COVID-19 and influenza have a similar disease presentation. They both cause respiratory disease, which presents as a wide range of illness from asymptomatic or mild through to severe disease and death. Secondly, both are transmitted by droplets spread through direct or close contact with an infected person, and indirect contact with contaminated surfaces, also known as fomite transmission.
The consequence of COVID-19 infection is more serious than seasonal flu, and therefore, it is important to understand more about their differences:
1. Both types of viruses can produce similar symptoms like fever, cough, headache, running nose, sore throat, fatigue, muscle and bone pain, diarrhea and even shortness of breath. However, in addition to the above-named symptoms, COVID-19 can affect taste, smell and produce inflammatory rash on the skin.
2. Both types of viruses can produce similar complications like sepsis, respiratory failure, lung fibrosis, heart inflammation, worsening of existing chronic diseases like diabetes and even multi-organs failures. COVID-19 can produce blood clot in veins and arteries of lung, heart, legs and brain. Moreover, it can cause a condition known as Multisystem Inflammatory Syndrome in Children (MIS-C). It is a condition where different body parts can become inflamed, including the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal organs. We do not yet know what cause MIS-C. MIS-C can be serious or even cause death. For COVID-19, existing data suggest that 80% of infections are mild or asymptomatic, 15% are severe infection, requiring oxygen and 5% are critical infections, requiring ventilation. These fractions of severe and critical infection would be higher than what is observed in influenza infection. The mortality rate of COVID-19 is about 3-4%, but it is less than 0.1% for flu. Therefore, we can see that COVID-19 is more hazardous than seasonal flu.
3. The epidemiology of flu and COVID-19 is different. The usual incubation period (the time from infection to appearance of symptoms) is about 3 days for flu and 5-6 days for COVID-19. However, the incubation period of COVID-19 can range from 2-14 days. The pre-symptomatic transmission (shedding of the virus before the appearance of symptoms) is a major driver of transmission for flu. In contrast, COVID-19 virus can shed virus 24-48 hours prior to symptom onset. At present, this does not appear to be a major driver of transmission. The infectivity of COVID-19 (Ro) is about 2-2.5, that means one patient can infect 2-3 people, which is higher than flu. However, the estimation for both COVID-19 and influenza viruses are very context-specific and time-specific, making direct comparisons more difficult. It appears that COVID-19 can produce more super-spreaders than flu. Therefore, we can see that the infectivity of COVID-19 is higher, but the transmission time is faster in flu.
4. COVID-19 virus attacks more adult than children but the condition is reverse in flu. In flu, the usual target patients are children, pregnant ladies, elderly, patients with chronic diseases (like diabetes and heart and lung diseases) and immune-compromised patients. The target groups of COVID-19 are the elderly and patients with chronic diseases.
5. The treatment of flu is simple and straight forward: the use of approved anti-viral drugs and flu-vaccine. There are multiple licensed influenza vaccines produced annually to protect against the 3 or 4 flu viruses that scientists predict will circulate each year.
6. There is no definite and internationally recognized and agreed treatment of COVID-19 at the moment. Various drugs including herbal medicines are used in different countries and the results are quite different. National Institute of Health (NIH) suggests a simple pharmacological protocol which may be useful for medical staff:
| Patient Condition | Suggested Treatment |
Not Hospitalized or Hospitalized but does not require supplemental oxygen | No pharmacological treatment Not recommend Dexamethasone (AI)* |
| Hospitalized and require supplemental oxygen | Remdesivir (AI)* or Dexamethasone If cannot take Remdesivir (BIII)* or Remdesivir + Dexamethasone (BIII)* |
| Hospitalized and require high flow rate oxygen delivery or non-invasive ventilation | Dexamethasone + Remdesivir (AIII)* Dexamethasone (AI)* |
| Hospitalized and require invasive mechanical ventilation or ECMO(External heart-lung machine) | Dexamethasone (AI)* Dexamethasone + Remdesivir (CIII)* |
*(A=strong evidence, B=Moderate, C=Optional)
*(I=High level evidence, II-Moderate level, III-Low level)
7. The vaccine for COVID-19 is under development. Readers can refer to our previous blog for vaccine development. Since we cannot check COVID-19 virus by clinical examination, the only method is to conduct a laboratory test as soon as possible. People should follow local health guidelines, monitor their symptoms and seek medical care in case of severe illness. Social distancing is very important to reduce the spread of COVID-19 virus. As the world is facing COVID-19 pandemic, the healthcare system is under great pressure. Taking flu vaccine can ease the burden of our healthcare system.
Dr. Jimmy Chan,
President of HK Association for Conflict and Catastrophe Medicine.
FHKAM(Surgery), FHKAM (Emergency Medicine)
Regional Director (HK), Advanced HazMat Life Support International, USA.
References:
1. Coronavirus disease (COVID-19): Similarities and differences with influenza, World Health Organization, 17 March 2020
2. Similarities and Differences between Flu and COVID-19, Centers for Disease Control ad Prevention
3. Guideline on COVID-19 Treatment, National Institutes of Health, 18 November 2020
4. Therapeutic Management of Patients with COVID-19, National Institutes of Health, 9 October 2020
5. Olsen SJ, Azziz-Baumgartner E, Budd AP, et al. Decreased Influenza Activity During the COVID-19 Pandemic — United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1305–1309. DOI: http://dx.doi.org/10.15585/mmwr.mm6937a6
6. Double threat of COVID-19 and influenza, The Lancet Respiratory Medicine, 22 October 2020
7. Double virus trouble: When COVID-19 meets the flu season, Al Jazeera, 7 October 2020

2020年11月17日
油麻地廣東道一幢唐樓在不久前發生火災, 多名居民吸入大量濃煙及慘遭火燒,場面觸目驚心, 導致7人喪生, 10多人傷, 震動全城, 是9年來最嚴重一次。大家還記得1996年11月20日在嘉利大廈發生的大火? 這場五級火警列作特別重大事故,造成41死80傷, 是香港歷史上最嚴重的高樓大廈火災, 亦是香港自1963年以來死亡人數最多的火災, 事發期間香港傳媒大篇幅報道, 而被困人士在高空躍下逃生及被烈火吞噬的畫面, 震撼整個香港社會。

圖片來源: 立場新聞
據了解, 大火可以在三分半鐘內達致攝氏600度高溫, 同時室內亦會濃煙密佈, 伸手不見五指, 難以辨別方向, 加上缺氧而導致呼吸困難、頭暈、心跳加速, 會令人極度驚恐, 如果未能保持鎮定逃離災場, 便會葬身火海。
要在大火中避免葬身火海, 唯一的方法就是盡快逃離現場,最好能跑到空曠的地方。傷者一方面要和時間競賽, 另一方面又要攻破各種逃生的障礙, 這些障礙包括火焰、障礙物件、高溫、濃煙和氧氣不足。大火需要氧氣才能燃燒, 所以關上防煙門, 減少氧氣的輸入, 便可以大大減低火災蔓延的速度。根據美國 Michigan 密歇根州立大學的研究, 大火會燃燒空氣中的氧氣, 導致傷者缺氧, 降低傷者逃生能力。
| 空氣中的氧氣濃度 | 人類的感覺 |
| 21% (正常空氣濃度) | 正常呼吸 |
| 17% | 判斷力及協調力下降 |
| 12% | 頭痛、頭暈、作嘔、疲倦 |
| 9% | 失去知覺 |
| 6% | 呼吸停止、心臟停止、死亡 |
根據國際不同防火機構的經驗, 在大火中導致死亡的主要原因不是火焰和燒傷, 而是吸入濃煙(有毒的氣體)而導致逃生困難, 現在很多家具都是採用合成纖維材料, 在大火中會釋放出大量的一氧化碳 (CO) 和氰化氫 (HCN, 山埃氣體), 一氧化碳會和身體紅血球結合, 阻礙紅血球攜帶氧氣供應細胞, 山埃會直接攻擊細胞內的線粒體(Mitochondria), 線粒體是能量工廠, 所以吸入濃煙便會很快導致缺氧和能量下降, 令傷者失去逃跑的能力而導致死亡。所以逃生的路線盡量要避免接觸濃煙, 才能增加逃生的機會。一氧化碳對空氣的比重為0.9670, 氰化氫對空氣的比重為0.941, 這兩種氣體都是比起空氣輕, 都會浮在濃煙的上層, 所以消防處建議若置身濃煙逃生的環境, 傷者最好是趴在地上逃走, 減少吸入一氧化碳和氰化氫的機會。
在發生火警時, 一方面要保持鎮定, 另一方面要和時間競賽, 不要浪費時間去攜帶貴重的物件, 細小的火可以嘗試用滅火筒撲滅。 如果遇上大火, 要盡快大聲呼叫通知鄰居逃生, 並且立即打999電話報警, 還要敲破火警玻璃啟動警鐘、自動灑水系統和緊急照明設備, 通知其他住客逃生。 出門逃生之前, 要帶備三樣重要的物件: 手提電話、大門鎖匙和掩蓋口鼻的濕毛巾。 開啟大門前,要用手感應大門的溫度, 如果大門很熱(特別是開門手柄), 表示外面有大火, 要小心判斷能否在這個時候開門逃生。 逃生的路徑要盡量避免接觸大火和濃煙, 不要使用電梯, 如判斷能衝得過便盡量趴低爬行, 減少吸入有毒氣體, 並沿途關上防火門阻止火警的蔓延, 如果衝不過,便要用鎖匙進回屋內, 選擇一個有窗的房間 (最好有兩門緊閉的緩衝區阻擋火勢蔓延進入), 還要找尋膠紙和濕毛巾, 將門的罅隙封住, 減少濃煙入侵。 在房間而可以打開少少窗戶幫助呼吸和揮動顏色布條呼救。
要粗略計算嚴重燒傷者的死亡率, 可以用一個簡單的方法:就是年歲加上傷者嚴重燒傷的身體面積, 傷者一隻手掌的面積大概是身體的1%,一個70歲20%嚴重燒傷的的傷者的死亡率大約是90%, 反之一個20歲20%嚴重燒傷的的傷者的死亡率大約是40%,。 如果身上著火, 要盡快將著火的衣物脫去, 或用大的濕毛巾將火蓋熄, 在地上慢慢滾動壓熄火焰也是一個方法。 奔跑只會增加火的威力, 因為這情況就好像在燒烤爐吹風一樣。
緊記預防勝於治療, 保護自己和他人的最好方法就是防止火警的發生, 建築物內不要儲存危險易燃物品, 檢查家居電器設備有沒有漏電情況, 小心火種特別是 不要在床邊抽煙。逃生通道要保持暢通, 經常檢查防火設備: 包括消防水缸、救火水喉、警鐘、自動灑水系統和緊急照明系統。制定逃生路線和在當眼的地方貼上逃生路線圖, 逃生路線最好是往下走到戶外的地方, 其他的選擇包括大廈的防火層和天台空曠的地方。有了防火設備, 有了逃生路線, 還需要定期的走火警演習, 演習時可以考慮蒙上眼睛, 模擬在大火中看不到環境的情況,加強真實感。如果能夠採用上述的措施, 在火警中能夠成功逃生的機會便會大大增加。
陳德勝 醫生
香港危難應變醫學會主席
美國亞利桑那大學高級核生化生命支援課程 香港區總監 (AHLS)
參考資料:
1. What Should I Do in the Event of a House Fire?, Safewise, 30 September 2020
2. How to Escape a House Fire?, PuroClean, 15 November 2019
3. What to do in a house fire, Fire and Emergency New Zealand Government, 2020
4. What to do if there's a fire, nidirect
5. High-Rise Fire Safety Tips, National Fire Protection Association
6. Smoke inhalation is the most common cause of death in house fires, Michigan State University, 28 January 2015
7. Home Fire Facts, Fire Department of San Francisco
8. House fires kill more Australians than all natural hazards, Macquarie University 10 September 2019

陳婉玲
根據香港政府統計處在2013年的統計調查[1],殘疾人士與智障人士數目超過65萬人,隨著香港人口逐漸老化,估計現時人數已遞增了不少。殘疾人士包括視障、聽障、肢體傷殘、智障、器官殘障/長期病患、言語障礙、自閉症、精神病、注意力不足/過度活躍症及特殊學習困難人士,雖然他們有一些限制和缺陷,但也有自身能力及潛能,與其他市民一樣,是社區重要的成員及持份者。
由於年齡的增長,很多人或身邊的親友,也有可能出現一些因疾病而成為殘疾人士;而每個社區/樓宇或多或少也會有殘疾人士居住,在防災及日常生活的需要上與大家息息相關。要預防災難發生和及時應變,大家的參與及協作,至關重要。
在香港,常見的災害包括火災、颱風、暴雨致水浸或山泥傾瀉、傳染病等,其中尤以火災最防不勝防,且隨時有可能發生,故每個家庭及每個社區,都必須有防災準備及計劃,萬一發生緊急事故,在消防員還未到達時,已能安全逃生,減低生命和財物的損失。
其實我們每個人在社會上也擔當著多個不同的角色,在防災備災計劃上,可以做得更周全,大家互相幫助,社區便更為安全。以預防家居火災為例,除了做好個人/家庭層面的預防措施,包括正確使用電器、爐具及易燃物品、預備好逃生包(內有重要證件、財物、手提電話、藥物…) 等之外,我們在其他角色上也可以做多幾步,作出貢獻:
- 住戶(包括殘疾人士): 主動與鄰居建立關係,守望相助,發生火災或緊急情況時,輔助有行動困難的鄰居一同撤離。
- 業主立案法團/物業管理公司成員: 訂立緊急事故應變計劃,並預先與住戶訂立緊急事故應變計劃,建立電話發佈訊息渠道(短訊/WhatsApp)予住戶,亦可為有特別需要的住戶建立關顧網絡,遇有火災或緊急事故時,能立刻發出訊息及致電通知住戶逃生,提高緊急撤離的效率。
社區的防災備災工作,除有賴政府部門做好相關工作、宣傳教育及救援計劃,以及非政府組織推廣防災教育工作外,市民理解殘疾人士的需要、大眾的防災態度及積極參與均非常重要,期望大家能共同攜手,構建更具包容性的安全社區,防備災難,保障生命。
參考資料:
[1] 2015年1月香港統計月刊, 香港政府統計處, 2015年1月
陳婉玲 (Elaine Chan)
曾於本港及海外從事災難管理及人道工作/項目多年,包括前線救災行動、災後重建、殘疾人士復康中心、備災減災、救災及醫療機構能力建設項目和相關人員培訓等,曾參與的災難項目包括地震、風災、水災、火災、傳染病爆發等。
[本文只供英語版本]
[本文只供英語版本]
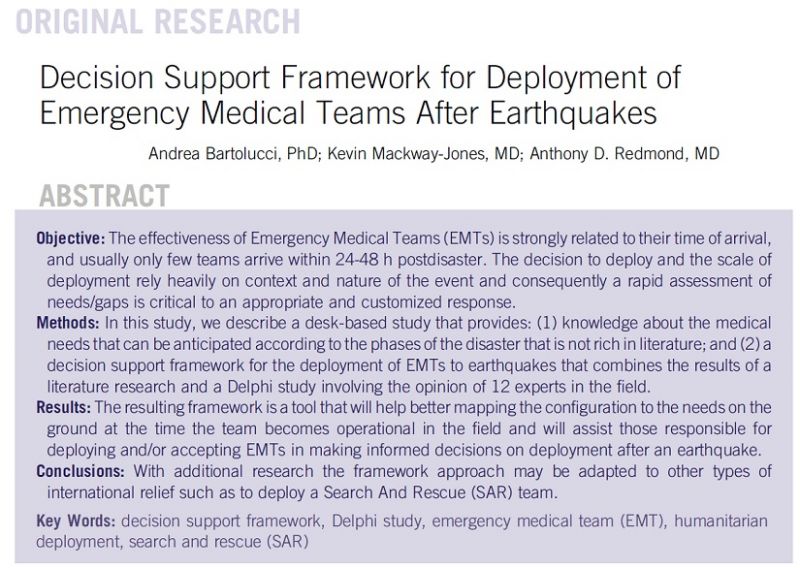
In times of Sudden Onset Disaster (SOD), timely emergency medical services are crucial to the affected communities. Being seen as one of the most important approach in emergency situations, emergency medical teams have a long history of responding to SODs such as the Haiti earthquake, the Indian Ocean Tsunami and the floods in Pakistan.
The World Health Organization has launched the Emergency Medical Teams (EMTs) initiative, formerly known as Foreign Medical Teams (FMTs) initiative, to introduce a classification, minimums standards and a registration system for EMTs that may provide quality healthcare services arriving within the aftermath of a SOD. The initiative historically focused on trauma and surgical needs, but outbreaks in Africa (Ebola) and Asia (diphtheria) have shown that EMTs’ responses are also valuable in responses to outbreaks and other forms of emergency which exceed the capacity of the local health system. [1]
SODs like earthquakes could cause mass casualty, and the surge in the needs for healthcare services could evolve within days, if not hours. In the article titled “Decision Support Framework for Deployment of Emergency Medical Teams after Earthquakes”, Bartolucci et. al. has summarized the evolvement of health needs in earthquake situation and observed that emergency surgical conditions reduced by 50% within the first week after the onset of the earthquake. The number of trauma cases dropped to less than 10% after 15 days.
According to another report published by WHO and the International Federation of Red Cross and Red Crescent Societies (IFRC) in 2017, The Regulations and Management of International Emergency Medical Teams [2], the timing of deployment (the time that the EMT is ready to attend to its first patient) in most of the SODs was not recorded properly. The study summarized some available data of several recent emergency operations, and has shown that the timing of deployment could vary from 2 days to 18 days. Yet in an emergency, the healthcare needs on ground may have changed drastically after 18 days.
Bartolucci et. al. continued to summarize experts’ opinions with a Delphi study followed by literature search and created an evidence-based framework for EMT coordinators and decision makers. The framework targets to facilitate decisions making in the configuration and capacity of the EMT. It can also facilitate a better estimation on the potential needs on ground so that EMTs can provide a timelier and quality healthcare service to the affected communities.
The article and the decision-making framework are available in the link below:
Decision Support Framework for Deployment of Emergency Medical Teams after Earthquakes
Reference:
[1] Fact Sheet: Emergency Medical Teams (EMTs), World Health Organization, May 2019
[2] The Regulations and Management of International Emergency Medical Teams, World Health Organization (WHO) & International Federatio of Red Cross and Red Crescent Societies (IFRC), June 2017
Elaine FONG
Manager (Professional and Knowledge Management)
Hong Kong Jockey Club Disaster Preparedness and Response Institute
*This article originates from a research funded by the Hong Kong Jockey Club Charities Trust within the collaborative project “Training and Research Development for Emergency Medical Teams with reference to the WHO Global EMTs initiative, classification and standards” between the Humanitarian and Conflict Response Institute (HCRI) and the Hong Kong Jockey Club Disaster Preparedness and Response Institute (HKJCDPRI)”.