You are here
概要: Enablers and Barriers - Community Engagement in Public Health Emergency Preparedness
概要: Enablers and Barriers - Community Engagement in Public Health Emergency Preparedness
[本文只供英語版本。]
In the event of emergencies, all stakeholders are encouraged to have effective plans which aim at mitigating the social and economic disruption of entire communities. Hence broader community engagement is a key to successful disaster risk management and emergency response. However, there has not been an up-to-date summary of the existing evidence on the enablers and barriers to community engagement in this context.
What did the research involve?
The European Centre for Disease Prevention and Control commissioned a study where Ramsbottom et al. reviewed 35 relevant documents published between 2000-2016.
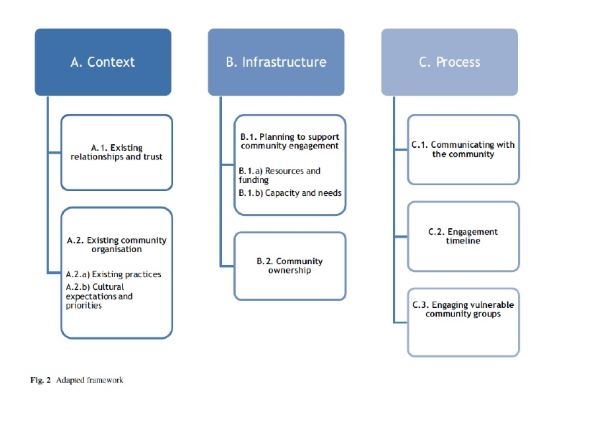
Based on an established framework of barriers and facilitators of community engagement in the public health domain1, they qualitatively analysed these documents and classified different factors into three broad aspects, namely “Context”, “Infrastructure” and “Process”.
What Did the Researchers Find?
Across the 3-phase Emergency Preparedness Cycle (EPC): Anticipation, Response, Recovery, most of the literature focused on community engagement during the anticipation phase, and findings were:
Trust between the communities and institutions is a prerequisite of successful engagement across all phases of the EPC. When designing emergency preparedness programme, it is important to consider local convention and practices, such as methods of obtaining information of decision-making. It is also crucial to understand local culture and value systems. For example, there may be competing priorities, such as social- or healthcare issues, that prevent communities from engaging in emergency response preparedness.
It would be favourable to start by identifying local capacities (e.g. networks of mutual support) and needs to inform planning and prioritisation. Appropriate community empowerment, which would enhance their sense of ownership, would facilitate effective community engagement. In particular, a decentralised approach to allow communities to lead in some planning activities (e.g. identifying priorities) would incentivise sustained action and involvement. Hence, flexible funding allocation is especially favourable, because it could facilitate the development of locally relevant partnerships and programmes.
To build engagement change over different phases of the EPC, communication methods should be tailored to:
- the demographics and cultural characteristics of different community groups across different stages;
- recognise the diversity of the community and dedicate special effort to engage vulnerable sub-population (e.g. linguistically isolated population); and
- ensure the delivery of coherent and consistent information to establish reliability and trust.
What Does it Mean?
Institutions should understand clearly their existing relationships with the targeted communities and reach out to build trust as the foundation of successful engagement.
While it is crucial to identify community-specific resources, needs, and enablers and barriers of engagement at an early stage, engagement should be made throughout the EPC by culturally competent staff, with special dedication to vulnerable groups.
The Way Forward
A two-way communication between institutions and communities should be in place to understand the needs and capacities of communities and promote a sense of ownership, and building a partnership between institutions and communities.
Finally, more research is necessary to understand the enablers and barriers to community engagement during the response and recovery phase of the EPC.
---------------------
1 IHHD. (2015). Review 5: Evidence review of barriers to, and facilitators of, community engagement approaches and practices in the UK. London: Institute of Health and Human Development.
This article is summarised from: Ramsbottom A, O’Brien E, Ciotti L, Takacs J. Enablers and barriers to community engagement in public health emergency preparedness: A literature review. Journal of community health. 2018 Apr 1;43(2):412-20.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5830497/pdf/10900_2017_Article_415.pdf